
views
Using Diet to Reduce Your Symptoms

Talk to your doctor or dietitian before you make changes to your diet. Making sudden changes to your diet will affect your gastroparesis, so visit with your doctor or see a dietitian to discuss your options. They’ll be able to help you come up with a diet that works for you and helps to ease the symptoms of your gastroparesis. Your doctor or dietitian can help you find new foods that will improve your symptoms.Tip: Finding the right diet for you is a process that takes time. As you make changes to your diet, if your symptoms seem to get worse or aren’t improving, contact your doctor or dietitian to discuss your options.
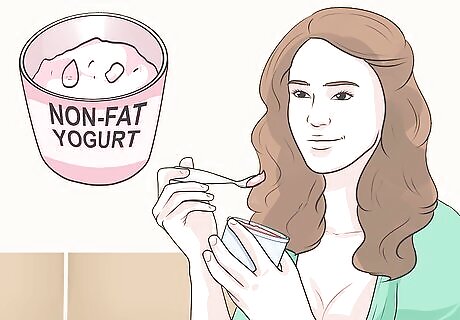
Eat foods that have a low fat content to speed up digestion. Because fat takes longer to digest, eating foods that have a high fat content will make your gastroparesis symptoms much worse. When you’re putting together your diet, choose low-fat foods to help improve your health and decrease your symptoms overall. Examples of low-fat food options include cottage cheese, Greek yogurt, egg whites, lean meats such as chicken or turkey breast, and fresh fruit. Avoid foods that are high in fat like red meat and cheese.
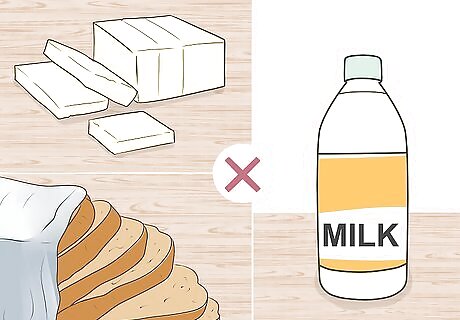
Limit foods with lots of fiber to improve your symptoms. Insoluble fiber is found in many foods and because it is more difficult for your body to digest, eating insoluble fiber will make your gastroparesis symptoms worse. Limit the amount of foods with insoluble fiber that you eat to a 1 serving a day, or avoid them entirely if you can. Insoluble fiber is found in whole wheat or bran products, green beans, potatoes, cauliflower, and nuts. Examples of foods that don’t have insoluble fiber include tofu, meat, dairy, white bread, and white rice. Because a low-fiber diet can cause constipation, and because fiber is an important part of a healthy diet, talk to your doctor before you cut out all foods with fiber in them.
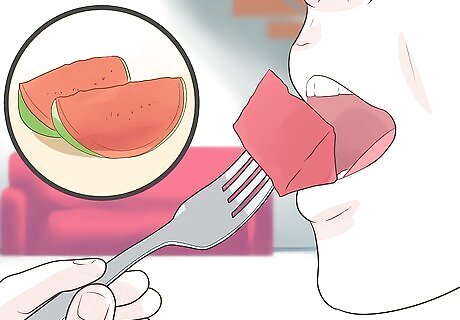
Choose foods that are softer and easier to digest. Select foods that are easy to chew and swallow and have a simpler structure so they’re easier for your stomach to break them down. Because gastroparesis affects your stomach’s ability to digest food, choosing foods that are easier to break down will make your symptoms less severe. A few examples of easy-to-digest foods include: White bread Soup Watermelon Peaches Pears Fruit juices Potatoes Apples without skin Mushrooms Lettuce Yogurt

Blend or puree your foods so they’re easier to digest. Blending your food turns it into almost a liquid, which means it will move through your stomach and digestive system faster, minimizing your gastroparesis symptoms. Use a blender to make tasty smoothies with fresh fruits and vegetables or blend your foods before you eat them. You can also purchase pureed fruit and vegetables for an option that’s easier to digest.
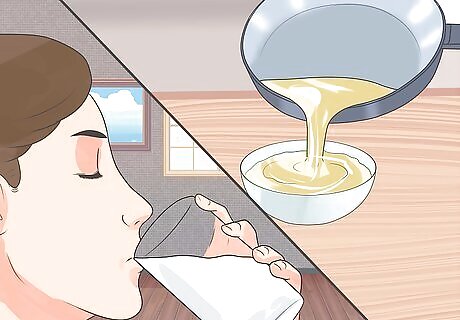
Get your nutrition from liquid sources as much as you can. Liquids such as protein shakes, juice, and soup are rich in nutrients as well as vitamins and minerals and are much easier to digest than solid food. Minimize your gastroparesis symptoms by including more liquids that are dense in nutrients. Be mindful of the fat content of nutrient-dense liquids so you don’t make your symptoms worse. Drink clear soups, broths, or sports drinks for their nutrients as well as their electrolytes.

Drink 1 cup (240 mL) of ginger tea a day to help with digestion. Ginger contains gingerol and shogaol, both of which aid in digestion and will ease your gastroparesis symptoms. Make a tasty ginger tea by bringing 1.5 cups (350 mL) of water to a boil, adding about 2 tablespoons (10 grams) of fresh ginger root, and letting it steep for about 10 minutes. Allow the tea to cool down a little before you drink it. If you don’t have fresh ginger, use dried.
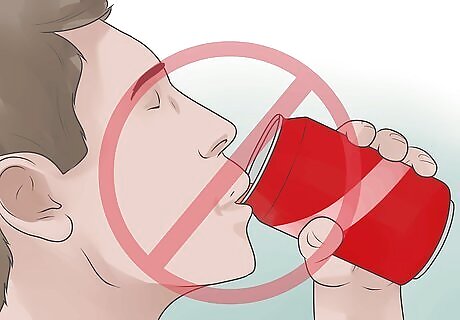
Avoid coffee, alcohol, and carbonated beverages. Coffee and alcohol will make your gastroparesis symptoms much worse. Carbonated beverages such as soda contain lots of air, which affects digestion and will exacerbate your gastroparesis symptoms. Avoid drinking them entirely to help reduce your symptoms.
Aiding Digestion

Chew your food thoroughly before you swallow to make it easier to digest. Chew your food until it’s almost liquid and there aren’t any lumps in it. For softer foods such as berries of cooked vegetables, break them up by chewing them 5-10 times. For tougher foods such as meat, start breaking them down by chewing each bite up to 30 times so it’s easier on your digestive system, which will reduce the symptoms of your gastroparesis. Taking the time to count your chews can force you to chew your food enough.
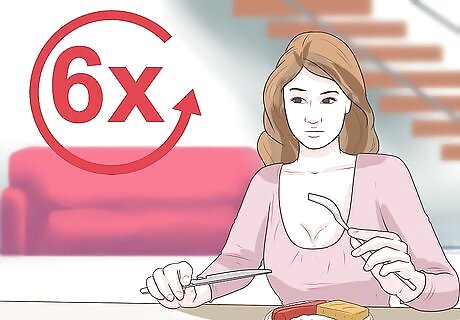
Eat 5-6 small meals to minimize stress on your digestive system. Eating 2-3 large meals a day is taxing on your digestive system and will increase the severity of your gastroparesis symptoms. Eat multiple, smaller meals throughout the day so your stomach doesn’t have to produce as much stomach acid or work as hard to digest your food, which will help with your symptoms. Focus on small, but nutritionally dense meals that don’t include lots of fat or fiber. For example, Greek yogurt with some fresh berries could be a great small meal. Did you know? Eating smaller portions throughout the day will also keep your blood sugar levels more constant and help with food cravings, which can help you maintain a healthy weight as well!

Go for a light walk after you eat to help digest your food. Exercise boosts your metabolism and will also help move food through your stomach and digestive system, which will make your gastroparesis symptoms feel better. When you finish a meal, take a short 10-15 minute walk to help your body process it. Don’t overexert yourself or do intense exercise after you eat or you could make your symptoms worse.

Avoid lying down for 2 hours after you eat. Lying down makes it more difficult for your stomach to process the food that you eat and will make your symptoms worse. After you finish a meal, give your body enough time to process it and empty your stomach before you lie down on the couch or in bed.

Quit smoking or avoid secondhand smoke so you don’t irritate your stomach. Smoking causes damage to your stomach lining and affects your digestion, both of which will exacerbate your gastroparesis symptoms. If you do smoke, quit as soon as you can to improve your symptoms. If you’re around others who smoke, try to avoid breathing in the secondhand smoke.
Knowing When to Seek Medical Treatment
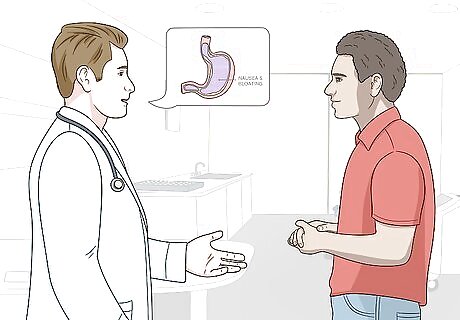
See your doctor for a gastroparesis diagnosis. The symptoms of gastroparesis can mimic a variety of other conditions, so see your doctor to get confirmation of what’s causing your symptoms. They can also help identify and treat any underlying issues that might be contributing to your gastroparesis, such as diabetes or an infection. Your doctor may conduct a variety of tests to determine if you have gastroparesis. One common test is the gastric emptying study, in which you consume food mixed with a small amount of radioactive tracer material, which can then be traced through your digestive tract. Your doctor may also perform an endoscopy, in which a tiny camera is passed into your stomach and small intestines through your throat to look for signs of gastroparesis or other conditions, such as peptic ulcers. Ultrasounds and stomach X-rays can also be useful tools for diagnosing gastroparesis.

Consult your doctor if dietary changes aren’t working. If you’ve been treating gastroparesis with diet and lifestyle changes and your symptoms aren’t getting better, see your doctor. They can recommend additional or alternative treatments that may help. For example, if you have severe nausea and vomiting, they can prescribe anti-nausea medications, such as prochlorperazine (Compro) or diphenhydramine (Benadryl). Other medications, such as metoclopramide (Reglan) or erythromycin, can help stimulate the movement of your stomach muscles. Talk to your doctor about the potential risks and side effects of these medications. For extremely severe cases of gastroparesis that prevent you from eating or drinking altogether, your doctor may recommend implanting a feeding tube or using a gastric venting tube to help reduce pressure in your stomach.
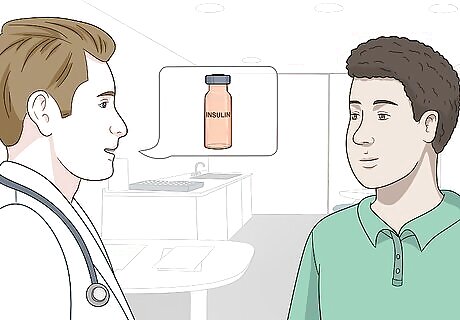
Create a treatment plan with your doctor if you have diabetes. Diabetes is a common cause of gastroparesis. Unfortunately, gastroparesis can often contribute to further complications with your diabetes, such as unpredictable changes in your blood sugar. To prevent potentially serious problems, you’ll need to work closely with your doctor to manage both your diabetes and your gastroparesis. Your doctor may recommend changing your insulin schedule in order to manage your blood glucose levels better. For example, they might recommend taking insulin more often or giving yourself injections after meals instead of before. You may also benefit from additional medications to help you manage your gastroparesis.
Call your doctor right away if you have symptoms of a bezoar. A bezoar, or a large mass of hardened, undigested food in your stomach, is a rare but potentially dangerous complication of gastroparesis. While most bezoars don’t cause any symptoms, sometimes they can block the passageway between your stomach and small intestine and cause serious digestive problems. See your doctor as soon as possible if you experience symptoms such as: Bloating Cramps Loss of appetite Nausea and vomiting Unexplained weight loss Symptoms of intestinal bleeding, such as bloody, red, or black stools


















Comments
0 comment