views
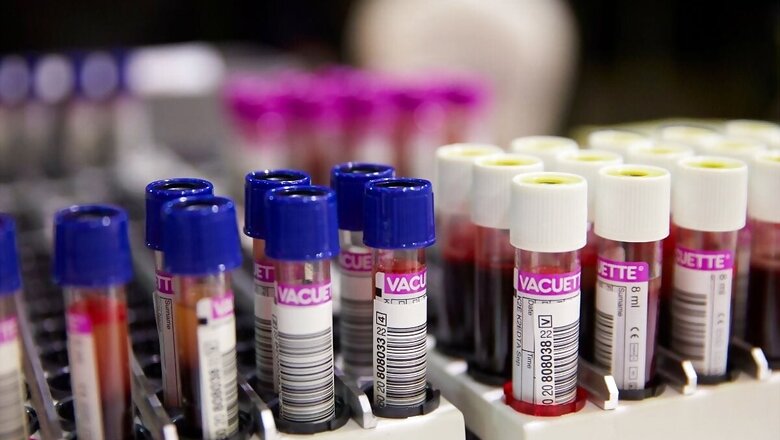
In today’s column, haematologist Dr Divya Bansal who is also a consultant at clinical haematology in Manipal Hospitals in Delhi, explains how patients who have recovered from Covid-19, especially the elderly, face the risks of cardiovascular complications and blood clotting.
In an interview with News18, Dr Bansal said that the COVID-19 pandemic that has affected billions around the world could not only cause life-threatening complications during the active infection but also has distressing after effects, some of which could be related to the blood. “As far as haematological aspect is concerned, post-discharge blood clotting in veins and arteries which sometimes may involve vital organs and sudden fall in blood counts especially platelets are the two major complications encountered in post-Covid patients,” she said.
Recent studies have shown that there is an increased risk of blood clotting, both arterial and venous, up to three months after discharge from Covid infections. The risk is higher among the elderly, patients with cardiovascular risk factors, those who have chronic kidney disease, patients with a previous history of blood clotting, those with underlying disorders of blood clotting and those admitted to ICU during active infection.
“Mild decrease in platelet count or thrombocytopenia has been seen not only during active infection but also may occur or continue up to six months. Most of these patients do not need any treatment as they are asymptomatic. Few patients may develop severely low platelet count and bleeding manifestations like skin bleeds, bleeding from the nose, gums or blood in urine or stool. These are the patients who will require treatment,” the doctor said.
Dr Bansal explained that many other haematological problems like low white cell count or low haemoglobin or bone marrow suppression post-Covid have been seen but are very infrequent complications. “Blood clotting incidence can be significantly decreased by continuing anticoagulation in high-risk patients post-discharge up to three months, but a regular follow up is mandatory, as there is a risk of bleeding in these patients,” said Bansal.
“Most of the patients with low platelet count have a mild fall in platelet count and are asymptomatic. These patients can be kept under close observation, and platelet count may recover spontaneously. Patients with severe thrombocytopenia and bleeding need specific treatment, as a most common cause of low platelet is immune destruction of platelets, most used treatment is intravenous immunoglobulins as it is non-immunosuppressive,” she added.
Read all the Latest News, Breaking News and Coronavirus News here.



















Comments
0 comment