views
India now has five Omicron cases as a person lodged in Delhi’s LNJP hospital as a suspected patient was confirmed to be infected with the newly emerged coronavirus variant on Sunday. The country’s first two cases were reported in Karnataka, and one case each was confirmed in Gujarat and Maharashtra. Since the onset of the variant in the world and India, authorities have been in a flurry to initiate strict Covid curbs, and travel restrictions. However, another important element to preventing the spread of any variant is contract tracing.
Since the pandemic began, a variety of variants have emerged, necessitating authorities to trace the contacts of a positive patient, to make sure other probable people infected with the virus don’t increase spread of the disease. Simply put, it is the process of attempting to identify people who have recently had contact with someone who has been diagnosed with an infectious disease in order to treat or quarantine them.
However, as simple as it sounds, different countries have different ways of tracing a person’s contacts to track the spread of disease. These involve lengthy algorithms followed by authorities on ground. In India, the National Centre for Disease Control (NCDC) also lays down its protocol for contact tracing.
According to the NCDC, since the SARS CoV-2 is a highly contagious virus, timely detection of contacts of a positive case is the “key to break the chain of transmission in the community”. The body recommends a dedicated unit for contact tracing and follow-up be established at the District level, with an identified Nodal Officer.
Steps for Contact Tracing, as Outlined by NCDC
1. Immediately after a confirmed case is identified, the case should be interviewed by the epidemiologist/medical officer. Details should be filled in the COVID-19 Case Investigation Form.
2. Attempt should be made to identify all the contacts (categorized above) household members, social contacts, contacts at work place and contacts in health care settings who have had contact with a confirmed case anytime between 2 days prior to onset of symptoms ( in the positive case) and the date of isolation (or maximum 14 days after the symptom onset in the case). Each contact/ place visited should be identified and recorded by the epidemiologist/medical officer. The list of contacts should be handed over to the front line health worker.
a. Example: if onset of symptom was of 24 March 2020, and the case sent for isolation on 29 March 2020, the contact tracing will be done from 22 March 2020 till date of isolation.
3. Based on information collected, the epidemiologist/medical officer should classify each contact as high-risk or low-risk.
4. Cases may have contacts in multiple states/UTs. The details of contacts living in different states should be immediately shared with the health authorities of the respective state with copy to national IDSP team. Tracking of contacts located in a state/UT will be the responsibility of that state/UT.
5. The contacts listed will be followed up by the FLW for the period of 14 days.
6. Testing of the contacts if indicated should also be captured. The contacts thus identified may be quarantined in dedicated facilities or at home depending on the norms of the State Government. In case of facility quarantine the reporting should be ensured by the facility in-charge.
For contacts quarantined at home, the following actions should be ensured:
1. It is vital that all the contacts are assessed everyday by the concerned team. The exact modality of assessment may be identified by the State Government.
2. During the initial assessment, the relevant instructions should be clearly communicated.
3. Help-line number should be provided to the quarantined contact with clear instructions on when to contact the health system.
4. The initial communication should emphasize on identification of early warning signs such as fever, respiratory symptoms, loss of taste/smell, etc. and immediate reporting to State helpline number.
5. If contacts refuse quarantine or monitoring, the supervisor/authorities should be notified.
6. At every opportunity effort should be made to identify any additional contacts that may have been missed previously. The added contacts will be updated in the master data base.
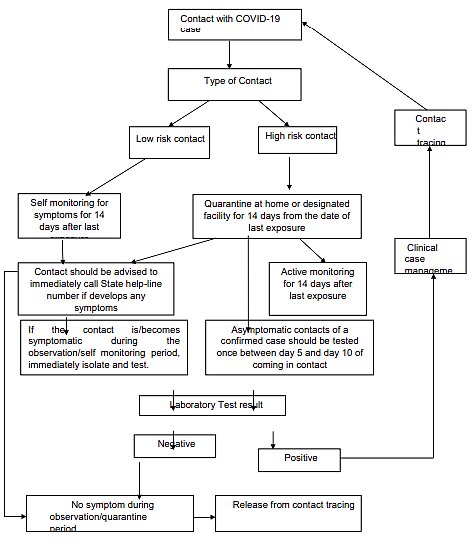
Algorithm for Contact Tracing:
(Courtesy NCDC)
Important considerations for Contact tracing
The decision to test some of the contacts and to quarantine others is based on risk assessment process considering factors like proximity, duration, nature of exposure as well as other factors, the NCDC says.
• A contact is a person who is likely to acquire infection from a positive case through any of the known modes of transmission.
• Anyone exposed to a symptomatic COVID-19 case, from 2 days before to 14 days after the onset of symptoms, if not isolated earlier.
• For asymptomatic or pre-symptomatic cases, the period for contact tracing is taken as 2 days before to 14 days after the date sample collection if not isolated earlier.
• The duration (more than 15 minutes), the proximity (more than one meter) and the nature (use of appropriate PPE), etc. of exposure are important considerations in contact tracing.
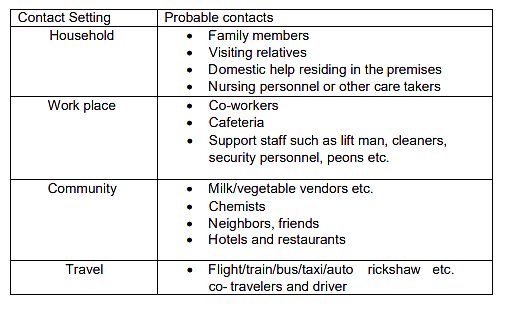
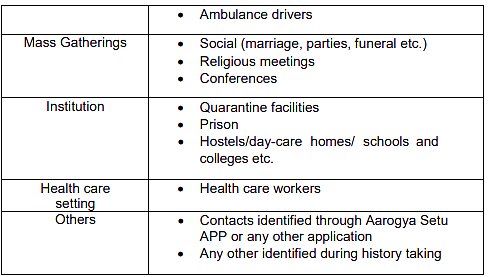
Who Can be Possible Contacts?
According to the NCDC, anyone from a person’s household to their workplace can be a possible contact of the infected patient. Milk vendors, chemists and fellow travellers can also be exposed to the virus. People in mass gatherings can also be contacts of a patient.
In Karnataka, authorities carried out tests of a 100 people who were part of a medical conference that the doctor who tested positive for Omicron had also attended. The patient had no travel history and authorities are using contact tracing also to determine where the patient could have possibly received the infection from.
High-risk Contacts and Low-risk Contacts
According to the guidelines of the body, there are two types of contacts: high-risk and low risk. These are determined on various factors; the contact’s continued proximity to the patient, wearing of masks or PPE or direct physical touch. The body also warns that low risk contacts do not mean ‘NO RISK’ contact; equal emphasis in
tracing must be given for low risk contacts as they may be potential sources for transmitting the infection.
1. High-risk contact:
• Lives in the same household as the case
• Anyone in close proximity (within 1 meter) of the confirmed case without precautions
• Touched or cleaned the linens, clothes, or dishes of the patient.
• Had direct physical contact with the body of the patient including physical examination without PPE.
• Passenger in close proximity (within 1 meter) of a conveyance with a symptomatic person who later tested positive for COVID-19.
• Touched body fluids of the case without appropriate PPE(respiratory tract secretions, blood, vomit, saliva, urine, feces)
2. Low-risk contact:
• Any contact not fitting into the above high risk contact description
Plan of Action for Contact Person:
High risk contact:
1. Quarantine at home or designated facility for 14 days from the date of last exposure.
a. Testing
i. If the contact is/becomes symptomatic during the observation period, immediately isolate and test.
ii. Asymptomatic contacts of a confirmed case should be tested once between day 5 and day 10 of coming in contact
b. While quarantined, active monitoring for 14 days after the last exposure.
c. Contact should be advised to immediately call State help-line number if develops any symptoms.
2. Remain reachable for active monitoring.
B. Low risk contact:
1. Should be advised for self monitoring for 14 days after date of last exposure.
2. They should be advised to use mask during the 14 day observation period and avoid crowded settings.
3. They should be advised to practice physical distancing, cough etiquettes and hand hygiene
4. Contact should be advised to immediately call State help-line number if develops any symptoms
5. They should be remain reachable during monitoring period.
Read all the Latest India News here


















Comments
0 comment