views
Getting Your Thyroid Surgically Removed
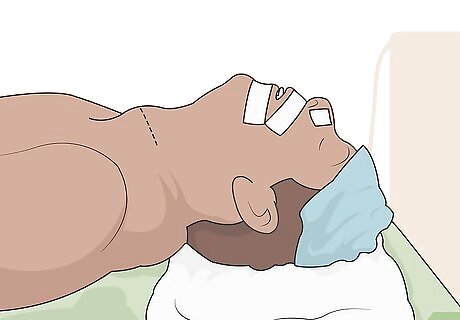
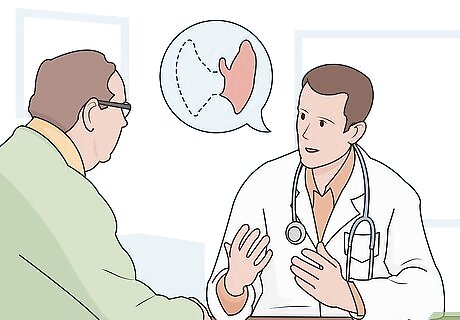
Get a thyroidectomy if your doctor recommends it. A thyroidectomy, or the surgical removal of most or all of your thyroid, is the most common treatment for thyroid cancer. Ask your doctor if they think you would benefit from having your thyroid removed. During a thyroidectomy, your surgeon will make an incision at the front of your neck near the base, just above your collarbones. They will remove your thyroid through this incision. Your surgeon may leave a small amount of tissue behind to avoid damaging the parathyroid glands, which are located at the back and sides of your thyroid. These glands help control the level of calcium in your body.
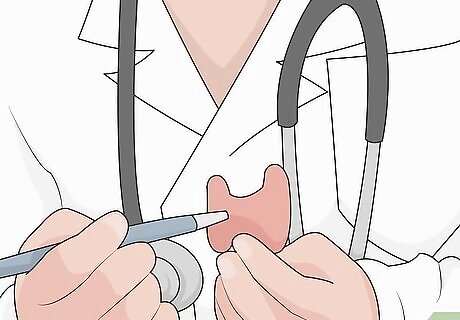
Discuss a lobectomy for smaller tumors. If you have a very small, well-defined cancerous tumor in your thyroid, it might not be necessary to remove the entire thyroid gland. Whether this type of surgery is appropriate will also depend on the type of cancer you have—for example, your doctor may recommend only a partial removal if you have a low-risk papillary cancer. Ask your doctor if you’re a good candidate for a lobectomy, in which only one side of the thyroid is removed. Some doctors will recommend a lobectomy if a fine needle biopsy isn’t enough to clearly diagnose your thyroid cancer. You may still need a complete thyroidectomy if the tissue from the lobectomy contains certain types of cancer cells (such as follicular cancer).
Ask if you will need any lymph nodes removed. In some cases, thyroid cancer can spread to the surrounding lymph nodes in your neck. If this has happened, your surgeon will need to remove any affected lymph nodes when they operate to remove your thyroid. If it’s not clear whether your lymph nodes are affected, your surgeon might still remove some during your thyroidectomy and test them for any signs of cancer.

Talk to your doctor about the potential risks of surgery. Any surgery comes with risks. Talk to your doctor about the possible complications or side effects of your surgery so that you know what to watch out for after your operation and when to seek medical attention. The common risks of thyroid surgery include:Warning: Call your doctor right away if you’ve had a thyroidectomy and you experience symptoms such as increasing pain, redness, or swelling at the incision site, bleeding from the incision, a fever of 100.5 °F (38.1 °C) or higher, difficulty eating or speaking, a persistent cough, or numbness or tingling in your face or lips. Excessive bleeding or an infection at the surgical site Damage to your parathyroid glands, which can cause a calcium deficiency Damage to the nerves connected to your vocal cords, which can affect your breathing or make it difficult for you to speak

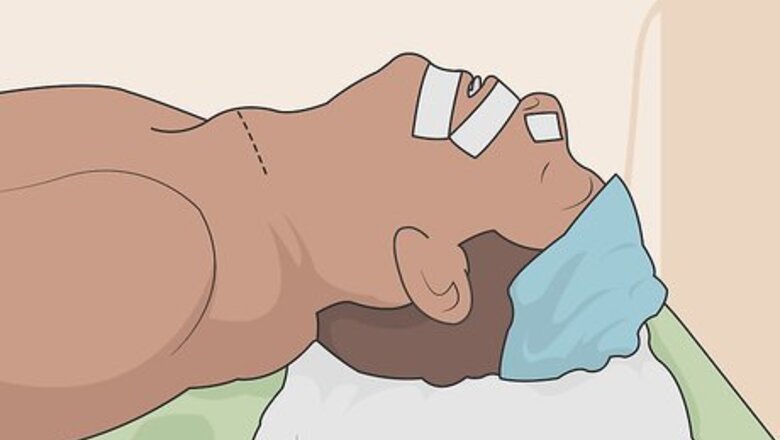
Follow any pre- and post-operative instructions carefully. Your surgeon will give you detailed instructions for how to prepare for your surgery and what to do during your recovery. Following these instructions will help keep you safe and ensure that the surgery is as successful as possible. Don’t hesitate to let your care team know if you have any questions or concerns about what to do. You will need to stop eating and drinking any foods or beverages a certain number of hours before the surgery. Your surgeon may also request that you shower or bathe before your surgery and avoid using skin-care products, such as lotions or perfumes. Your doctor will also tell you what to expect during your recovery and how long it will be before you can return to your regular activities. Follow their instructions about caring for your surgical site (such as whether you need to change the dressings and how to safely clean the area).

Take thyroid hormone medication after your surgery. Once you’ve had your thyroid removed, you’ll need to take replacement thyroid hormone medication for the rest of your life. Take the medication exactly as directed and check in with your doctor as often as recommended to make sure the dosage is still working well for you. The synthetic thyroid hormone is known as levothyroxine. Common brands include Synthroid and Levoxyl. It comes in the form of a pill that you will need to take on an empty stomach, typically first thing in the morning. Even if you’ve had only part of your thyroid removed, you may still need lifelong replacement hormone therapy. There’s a greater chance you’ll need hormone therapy if you have an underlying thyroid condition, such as Hashimoto’s disease.
Using Non-Surgical Treatments

Get radioactive iodine treatment to destroy remaining thyroid tissue. If your doctor is concerned that your cancer might return, or that surgery alone wasn’t enough to get rid of all of it, they may recommend radioactive iodine therapy. Swallow the iodine in the form of a capsule or liquid as directed by your doctor. This treatment is also helpful for more advanced cancers that may have spread beyond the thyroid. Radioactive iodine is relatively safe, since the radioactivity is almost entirely absorbed by your thyroid cells. However, you may experience side effects, such as nausea, dry mouth or dry eyes, fatigue, and changes to your sense of taste or smell. You may need to avoid close contact with vulnerable people, such as children or pregnant women, for a few days after treatment. The radioactive material will eventually leave your body through your urine.
Discuss external radiation therapy for cancers that return or spread. External beam radiation therapy involves aiming a concentrated beam of radiation at the cancerous tissue. Your doctor may recommend this treatment if your cancer doesn’t respond well to radioactive iodine or if it comes back after surgery and radioactive iodine treatments. This treatment is most commonly used for medullary and anaplastic thyroid cancers, which are less common and more difficult to treat than follicular or papillary thyroid cancers. You will need multiple radiation treatments, typically spread out over the course of 5 weeks. Common side effects include fatigue, dry mouth, trouble swallowing, and skin irritation similar to a sunburn at the site where the radiation was administered.

Ask about chemotherapy for hard-to-treat thyroid cancer. If your thyroid cancer isn’t responding well to other treatments, your doctor may recommend chemotherapy. This is a type of drug treatment that directly attacks cancer cells. Talk to your doctor about using chemotherapy in combination with other treatments, such as surgery and radiation therapy. Chemotherapy may be helpful for treating aggressive thyroid cancers that spread readily to other parts of the body, such as anaplastic thyroid cancer. If you have advanced thyroid cancer, your doctor might also recommend targeted cancer drugs, such as cabozantinib (Cometriq), sorafenib (Nexavar), or vandetanib (Caprelsa).Warning: Chemotherapy can cause severe side effects, such as hair loss, nausea and vomiting, diarrhea, decreased appetite, anemia, and increased vulnerability to infections. Talk to your doctor about the best way to manage these side effects.
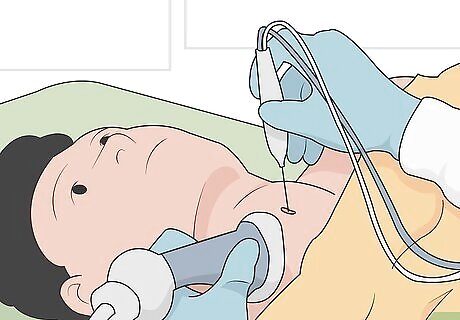
Use alcohol ablation to treat small cancers that can’t be reached with surgery. If you have small cancers that can’t be easily removed surgically, your doctor may be able to treat them by injecting alcohol directly into the tumors. They will use an ultrasound to guide the needle to the right location within your thyroid. This treatment can also be helpful for small, recurring thyroid cancers.
Managing Your Symptoms

Ask your doctor to recommend a palliative care specialist. In addition to treating the cancer itself, you’ll also benefit from treatments that help relieve your symptoms. Palliative care can help bring relief from both the symptoms of your cancer and the side effects of the treatments you receive. Ask your doctor to recommend a specialist who has experience working with thyroid cancer patients. Palliative care may include medications to manage your pain and relieve side effects from cancer treatments, such as nausea or loss of appetite. If you have trouble breathing or swallowing, you might also benefit from procedures like airway stenting or feeding tube implantation. In advanced cases or thyroid cancer, treatments like radiation or chemotherapy may be used to bring relief from your cancer symptoms even if they can’t fully eliminate the cancer.
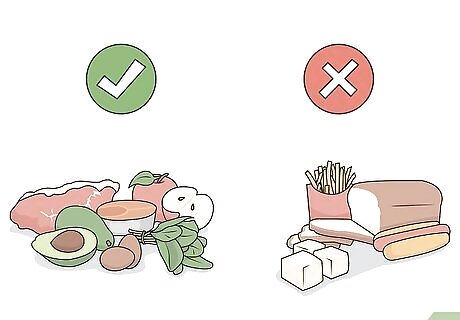
Eat a healthy diet to improve your overall health. You’ll feel your best during and after your thyroid cancer treatment(s) if you take good care of your body. Eat a balanced diet with plenty of fruits, vegetables, lean proteins, and healthy sources of fat to give yourself energy and promote healing.Keep in mind: Depending on your type of thyroid cancer and what treatments you’re receiving, your doctor may recommend a special diet. For example, you may need to temporarily reduce your iodine intake if you’re taking radioactive iodine.

Get plenty of sleep to help your body heal. Getting a good night’s sleep will help reduce stress, improve your energy levels, and boost your immune system. If you have trouble sleeping, talk to your doctor. They can recommend strategies or prescribe medications to help you sleep better. To help yourself sleep better, turn off all bright screens, such as TVs, phones, or computers, 2 hours before bedtime. Keep your room dark, quiet, and comfortable at night. You may find it helpful to unwind with a relaxing pre-bedtime routine, such as taking a warm shower, meditating, or listening to peaceful music.
Exercise most days of the week to manage stress and fatigue. Exercise is a great way to boost your energy and help you feel better overall when you’re dealing with cancer. Talk to your doctor about what kind of exercise is safe for you during and after your thyroid cancer treatments. If possible, try to get half an hour of aerobic exercise 3 days out of the week. Examples of aerobic exercise include walking, jogging, swimming, and cycling.

Join a thyroid cancer support group if you feel overwhelmed. Dealing with cancer is scary and stressful. If you feel like you need extra emotional support, joining a support group can help. Talking to other survivors can help you feel less alone and put your experiences in perspective. Ask your doctor to recommend a group in your area. You can also use resources like the American Cancer Society’s Cancer Survivors Network or the Thyroid Cancer Survivors’ Association.
















Comments
0 comment